Six of the seven days in the hospital were spent waiting for placement, not because she needed additional medical care or because rehabilitation beds were unavailable. This delay occurred because the process of matching a patient to the right post-acute facility (skilled nursing homes, rehabilitation centers, and similar settings where patients continue recovery), verifying insurance coverage, coordinating admission logistics, and finalizing the handoff remains shockingly manual and fragmented in 2025.
This discharge bottleneck impacts millions of Americans and costs our healthcare system billions every year.

Why Care Transitions Fail Today
I grew up in a family of clinicians. My grandfather helped discover EPO (a hormone critical to treating anemia), transforming kidney dialysis treatment. My mother is a psychiatrist. My brother is now following their footsteps in his third year of medical school. With this background, I grew up implicitly trusting that our healthcare system would have the tools to help me navigate the system should I ever need it.
Then, a few years ago, I saw my mother and her siblings take on a caretaker role for my grandmother. As she declined, it became increasingly clear that she could no longer live independently and needed full-time care. The process was excruciating: my mother, a doctor and more medically proficient than most, struggled to find an assisted living community that met both our family needs and my grandmother’s clinical requirements.
I watched someone with deep medical expertise and an insider’s knowledge of the system struggle to navigate this fragmented, information-poor process.
When Akash and I compared our families' experiences with discharge and post-acute placement, we started asking questions. Connecting patients to the right post-acute care is critical to patient outcomes and hospital operations, yet this process hasn't evolved in decades. We wanted to understand why.
Legacy Solutions for Hospitals Aren’t Cutting It
As we started having conversations, we spoke to numerous hospital executives, discharge coordinators, and case managers. We found that this process wasn’t just frustrating for the patients, but also was deeply challenging for the care teams that manage it day in and day out. We also discovered that the solutions leveraged today aren't solving the fundamental problems.
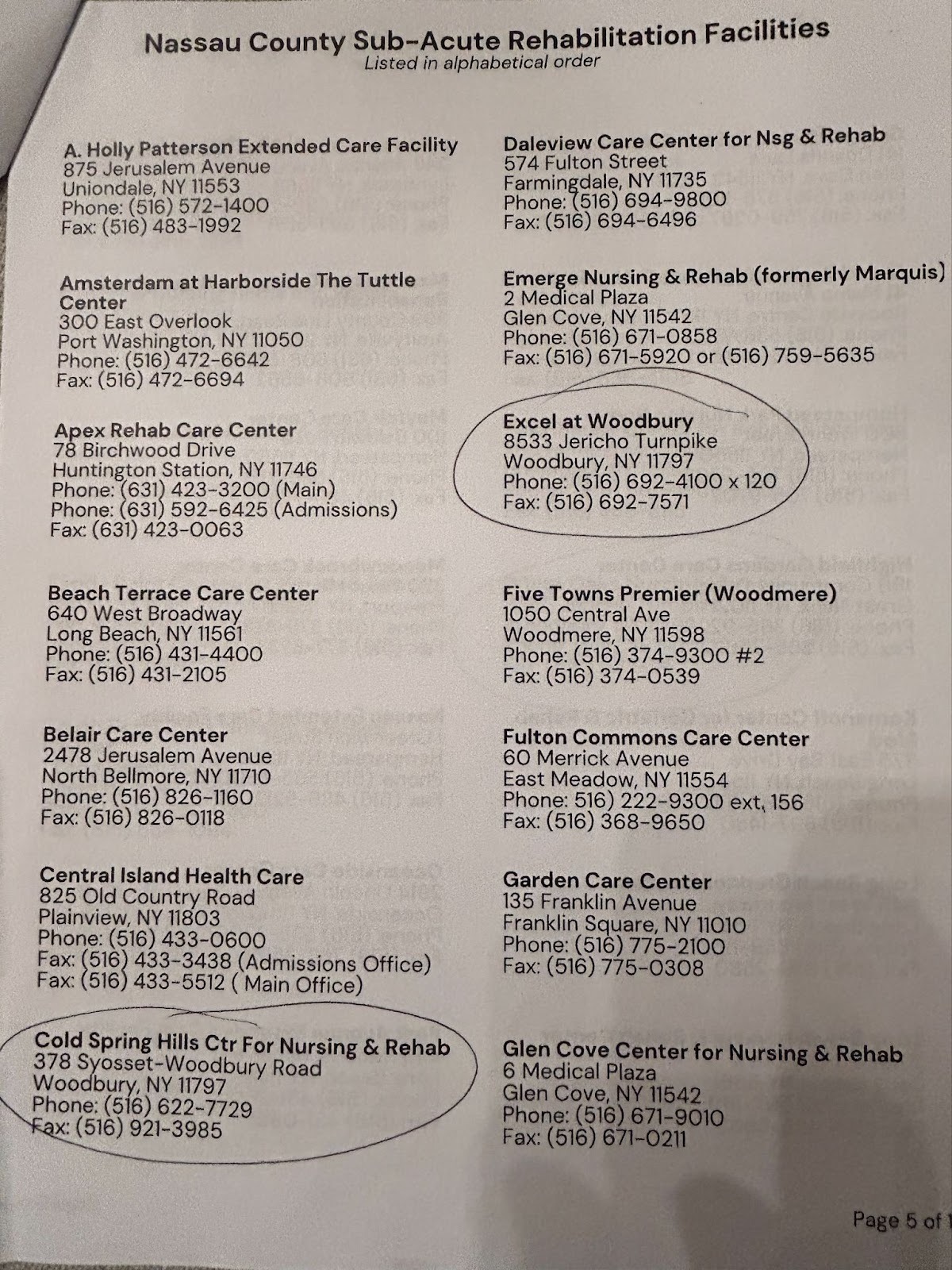
The technologies that are currently in use are e-fax solutions that do not address patient and family needs and still require considerable manual work to complete a referral. Families receive printed lists with facility names and little else, then are expected to make a decision that dramatically affects their loved one’s recovery. The Centers for Medicare & Medicaid Services (the federal agency that administers Medicare and Medicaid) mandates that the patient gets to make the choice, but doesn't mandate information quality or accessibility.
Once a family has indicated their preferred facilities, hospital discharge coordinators and case managers initiate the referral process to determine what facilities are equipped and have availability to accept the patient. On top of sending the official referral request through the e-fax, they will make 20-50 phone calls per patient to confirm basic information like bed availability, insurance acceptance, clinical capabilities, and admission requirements. Often, case managers spend hours battling payers over prior authorization appeals, all while the patient waits in an expensive hospital bed.
Post-Acute Care Challenges: Capacity, Authorization, and Coordination
In our quest to understand the status quo, we also spent time with post-acute facility owners, executives, and day-to-day operators to better understand their role in helping patients leave the hospital and move through their recovery.
From these conversations, we learned that post-acute care facilities rely on building direct relationships with hospitals to drive referrals and increase occupancy in their facilities. This approach can be effective, but is manual to build and maintain. These facilities are also increasingly burdened with challenging prior authorization and appeal processes that create barriers to accepting new patients and supporting their timely care transitions.
Newer solutions in the space are focused on automating intake-related tasks for post-acute care facilities, but do not tackle the bigger alignment challenges that exist with payers and hospitals to maximize occupancy and streamline intake workflows.
It’s Never Been a More Important Time to Streamline This Process
With the median hospital operating margin hovering at 1.2%, and recent legislative changes expected to compress hospital margins further, health system executives are looking for operational leverage wherever they can find it. They need to move patients through their facilities more efficiently, reduce readmissions, and maximize revenue per bed.
Post-acute providers face similar pressures. Although volumes have stabilized to their pre-COVID levels, post-acute margins are incredibly tight. There are headwinds, too: increasing friction from prior and re-authorizations creates additional overhead for post-acute care operators and forces them to make difficult referral decisions to keep business viable.
The result: an incredibly inefficient market where both sides lose. Patients and families deserve more, and we knew we could build something better.
Sonder Health: An AI-Powered Platform for Acute-to-Post-Acute Transitions
We're building Sonder Health to become the singular platform to connect every point of care across post-acute transitions. This platform will enable seamless coordination across the entire care continuum, making it possible for patients, families, clinicians, providers and payers to work together without friction.
We're starting with the acute-to-post-acute transitions because these referrals are for the highest-acuity patients, create the longest discharge delays, and generate the most readmission risk.
We believe we can transform transitions of care and referrals to post-acute by:
- Taking an AI-native, agentic approach to eliminate administrative work that previously couldn't be automated.
- Prioritizing and building for the family and patient experience. We believe this leads to faster referrals and better patient outcomes.
- Aligning incentives by driving more transparency between hospitals and post-acute care providers.
Through this approach, we can unlock hospital length of stay reduction and patient throughput that was not possible before. The opportunity is substantial: a 0.25-0.5 day reduction in length of stay for patients requiring post-acute care would improve hospital margins by >1%. We're building to deliver that impact.
Our long-term vision extends well beyond this initial focus. We're creating an updated technological and operational framework for how referrals should work across the entirety of the care continuum. This approach aligns incentives across health systems, post-acute care providers, patients, families, and payers, creating the foundation to rebuild trust in the system.
Meet the Team Behind Sonder Health
Akash and I have each spent our careers deploying enterprise technology at the largest health systems, provider groups, and value-based care organizations across the country. We've learned firsthand what it takes to build solutions that actually get implemented and drive value in complex healthcare environments.
We first worked together at Ribbon Health, scaling care navigation and referral management solutions that connected millions of patients to providers. We know how referral workflows operate and what it takes to build and scale enterprise-ready platforms.
But this isn't just professional expertise. When we compared notes on our families' experiences with the discharge bottleneck, the parallels were immediate: patients were stuck in hospitals not because of clinical needs, but because the systems connecting them to the next level of care suffered from the same types of breakdowns we'd addressed elsewhere in healthcare: fragmented data, manual coordination, and misaligned incentives. Those conversations became Sonder Health.
We believe we can build technology that challenges the status quo and sets a new standard for patient throughput and discharge navigation.
Help Us Build the Future of Transitions of Care
If you're a hospital executive who's been searching for better ways to manage discharge planning and reduce length of stay, we'd love to talk.
If you're a post-acute care leader tired of inconsistent referral flow and looking for more predictable census management, let's connect.
If you're a builder, engineer, or operator who wants to work on a problem that touches millions of patients every year, reach out.
The issues that arise during transition from one care facility to another are some of the most pressing problems in American healthcare. These transitions of care have been neglected for too long, and the consequences compound every day. We're here to build the solution that should have existed years ago, and we're doing it with the experience, the technology, and the partnerships needed to make it real. This is how we rebuild trust in healthcare, one successful patient transition at a time.
– Elizabeth Duffield | founders@sonderhealth.co


.webp)

